A new complication from treatment with bisphosphonates has become an important disease condition for the dental professional to recognize. Bisphosphonate-related osteonecrosis of the jaw (BRONJ) manifests itself as devitalized exposed bone in the maxillofacial region. Patients may be considered to have BRONJ, if all three of the following are presented simultaneously:
- Current or previous treatment with bisphosphonates.
- Exposed bone in the maxillofacial region for greater than eight weeks.
- No history of radiation to the jaws.
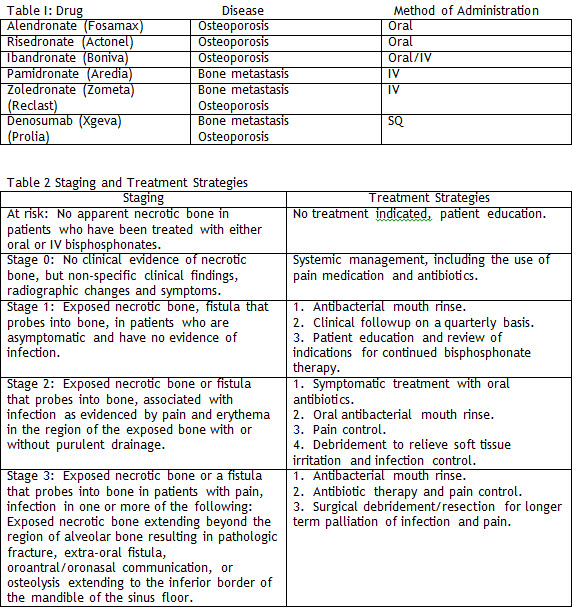
Bisphosphonates are used to treat osteoporosis and malignant bone metastases. These medications, oral and intravenous (table 1), inhibit bone resorption by suppressing the recruitment and activity of osteoclast. They typically have a very long half life. The precise mechanism that leads to BRONJ is unknown. It is hypothesized that bisphosphonates have an unfavorable influence on bone healing because of their suppression of osteoclastic activity. Additionally, bisphosphonates inhibit osteoblastic-mediated osteoclastic resorption and are antiangiogenic. These varied properties of bisphosphonates significantly interfere with the patients ability to heal in the face of local trauma such as extraction, fracture, or infection.
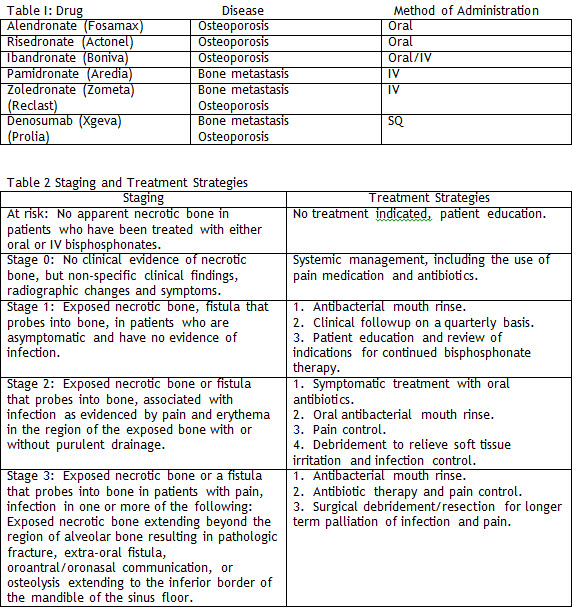
BRONJ appears to exclusively affect the jaws. It usually presents as an ulcer with exposed bone after extraction of tooth, or spontaneously (non-trauma or infection induced). Spontaneous bone exposure has been reported and may in fact represent the earliest stage of BRONJ (table 2).
Patients may be asymptomatic or have pain. Infection is also a common finding and may exacerbate the hard and soft tissue presentation. Purulence and swelling typically occur as the condition worsens. Dentition may be compromised.
Treatment objectives for the patient with BRONJ focus on elimination of pain, control of any infection, minimizing bone necrosis, maximization of soft tissue health, and maintaining excellent oral hygiene.
Areas of necrotic bone that irritate soft tissue should be removed and/or recontoured to promote soft tissue healing. Removal of symptomatic teeth in the involved area is recommended. Steps to promote wound healing such as hyperbaric oxygen and platelet-rich plasma are encouraged, although clinical data validating their positive contribution is lacking.
Dr. Lee (Mac) Whitesides, DDS, MMS is Board Certified in Oral & Maxillofacial Surgery. Dr. Whitesides is one of only two oral-maxillofacial surgeons in the United States who currently hold a Masters degree in Anesthesia and Oral Surgery. He has extensive experience with Distraction Osteogenesis for the Maxillofacial Skeleton, generating sufficient quantity of bone height and width to provide the appropriate foundation for Dental Implants.
©Copyright - All Rights Reserved
DO NOT REPRODUCE WITHOUT WRITTEN PERMISSION BY AUTHOR.